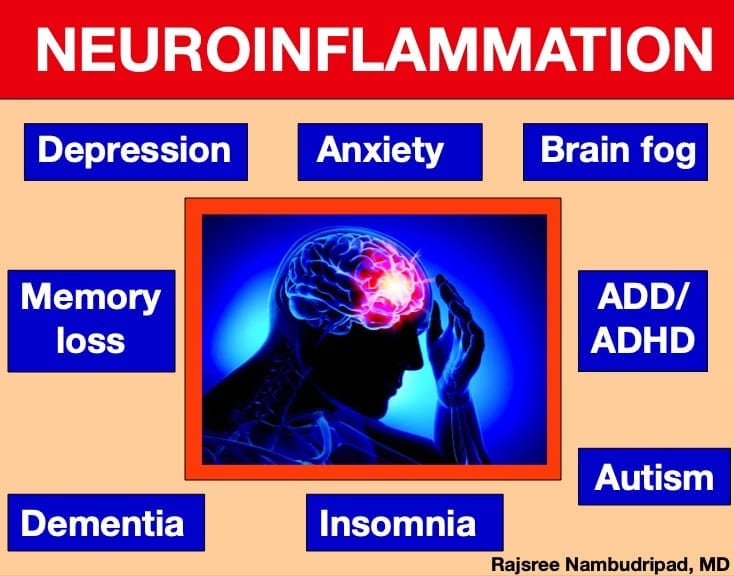
Our brain is our control center for our intelligence, mental sharpness and mood. Sadly, our brain can become inflamed. This is called neuroinflammation. Symptoms of neuroinflammation are definitely on the rise during the last few months coinciding with the changes in the world. Nearly half my patients are experiencing symptoms related to neuroinflammation such as anxiety, depression, brain fog, insomnia, and memory lapses.
The concept of neuroinflammation in psychiatry is now reaching mainstream medicine. Uma Naidoo, MD is a psychiatrist and professor at Harvard Medical School (Massachusetts General Hospital) and is now leading the research on the role of nutrition and the gut microbiome in mental health conditions. She also happens to be a professional chef, too! I highly recommend her recent book, “This is your Brain on Food.”
What are some causes of neuroinflammation?
1) Inflammatory diet — sugar, vegetable oils, processed foods, pesticides, chemicals and preservatives.
2) Gut inflammation — Leaky gut, bacterial imbalances (dysbiosis or SIBO), gut infections, parasites, exposure to food allergens and sensitivities. Remember, the gut is the “second brain.”
3) High cortisol — Cortisol is the “bad” stress hormone. Many of my patients are showing high cortisol levels in the last few months and exhibiting symptoms of anxiety, panic, and insomnia.
4) Nutrient deficiencies — Low vitamin D, low omega 3 fatty acids, low magnesium, low zinc, low B vitamins are common and easily correctable.
5) Toxins — This includes exposure to heavy metals like lead, mercury, arsenic, as well as exposure to mold. With more people working and studying from home (kids too!), brains are being exposed to larger amounts of EMF from constantly being in front of a screen.
6) Autoimmunity — We see this in patients with high levels of inflammation due to autoimmune conditions like Hashimoto’s thyroid disease, Lupus, Rheumatoid arthritis, and Inflammatory Bowel disease. As we heal the autoimmune process, inflammation in the body and the brain goes down.
7) Traumas — This includes both physical traumas (car accidents) as well as emotional traumas.
8) Slowed detox pathways — This is why I always measure homocysteine to get an idea of your methylation/ detox pathways. High homocysteine levels are associated with increased risk of depression, dementia, and Alzheimer’s disease. 50% of the population has a gene mutation in MTHFR which affects how they detox.
In my practice, I like to assess all the above factors in understanding symptoms of neuroinflammation. We take it step by step to address the diet, nutrient deficiencies, hormones, gut health, and detox pathways. As inflammation in the body goes down, so too does neuroinflammation. Mood and mental sharpness improve!
In these challenging times, we need to pay closer attention to our health, particularly mental health. Neuroinflammation is on the rise, but definitely treatable once we find and address the root cause.
Wishing you all great health,

Rajsree Nambudripad, MD











 Dr. Rajsree is a caring and compassionate physician, who is board-certified in both Internal Medicine and Integrative/Holistic medicine. She is passionate about helping patients optimize their health through a preventative approach involving healthy lifestyle, dietary changes, targeted nutritional supplementation, and optimizing hormones. Her practice is unique in the personalized attention she devotes to each and every patient.
Dr. Rajsree is a caring and compassionate physician, who is board-certified in both Internal Medicine and Integrative/Holistic medicine. She is passionate about helping patients optimize their health through a preventative approach involving healthy lifestyle, dietary changes, targeted nutritional supplementation, and optimizing hormones. Her practice is unique in the personalized attention she devotes to each and every patient.